Feature Stories
Protecting Pregnancy with Smartphones
Three leading institutions join forces to combat pregnancy-related complications and death
Women in the U.S. are more likely to die from childbirth or pregnancy-related causes than other women in the developed world. About 700 women die each year in the U.S. as a result of pregnancy or delivery complications.
Unlike other leading causes of death such as cancer or Alzheimer's disease, birth-related deaths are largely preventable. Today, however, most adverse pregnancy outcomes are not predictable, and thus cannot be avoided, partly because of a lack of medical data.
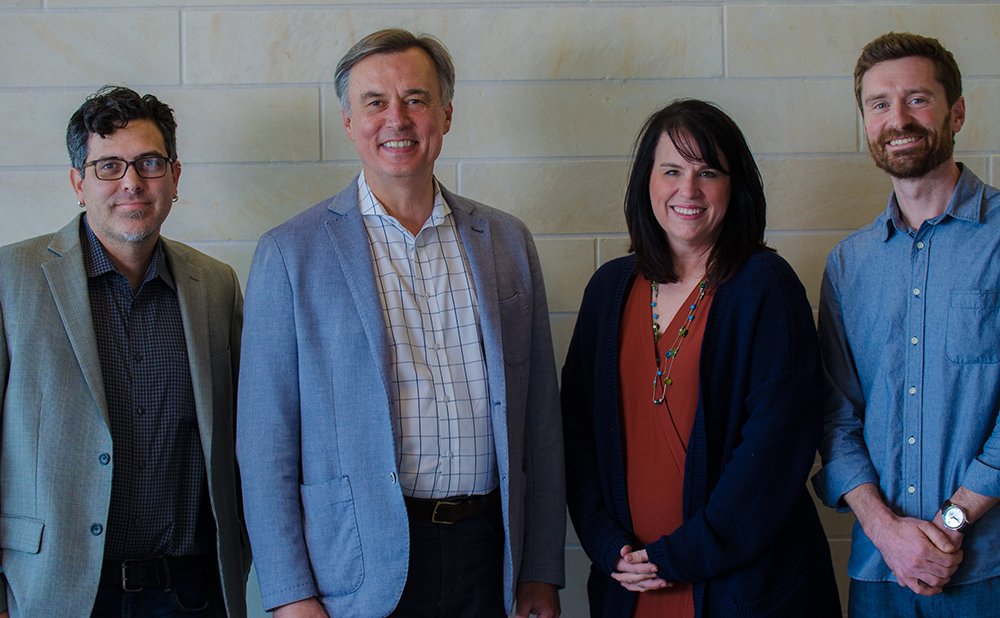
A newly-appointed team has brought together researchers and physicians from TACC, the Dell Medical School (Dell Med) Department of Women's Health, and the Institute for Computational Engineering and Sciences (ICES) at UT Austin. This team of experts is working to close the gap in medical evidence for complications such as maternal mortality, emergency C-sections, stillbirth, neonatal death, pre-term birth, and other important health issues.
In September 2018, the National Science Foundation awarded the team a $1.2 million Smart and Connected Health grant to support their research.
"We are very excited," said Radek Bukowski, a co-principle investigater (PI) on the grant and associate chair of Women's Health at Dell Med. "The project is innovative, full of promise, and unprecedented in the novelty of the approach."
Using smart phones, the team will passively monitor the activity and behavior of 1,000 pregnant women in the Austin area. The ultimate goal is to develop digital phenotypes, or profiles, to better understand factors that influence pregnancy and can inform individualized pregnancy care.
Participants will download a smartphone application originally developed at Harvard University and modified for this project to collect physical, social, and behavioral data. The app captures activity over time such as a participant's movement, interaction with their social network, typing speed, and screen time. Analysis of this large collection of digital data, in combination with traditional clinical data collected via participants' medical records, informs the development of a digital phenotype of pregnancy.
"From their first appointment to six weeks post-partum, we'll be able to analyze data to determine the impact of their everyday lives on their medical outcomes, and determine whether we see any digital markers of significant events such as labor," said Kelly Gaither, the grant's PI as well as director of Health Analytics at TACC and an associate professor for Women's Health with the Dell Medical School. "We can examine, for example, whether these women have an active social structure, changes in speech patterns, and unusual sleep patterns — even the number of steps they take in a day."
With the ubiquitous use of smartphones, it is now possible to collect lived experiences or data reflecting markers of pregnancy. "And the beauty of it is it's completely passive and unobtrusive collection," Gaither explained. "We can collect these behaviors, generically, without needing to collect sensitive data such as text messages and conversations."
Using computational technologies in obstetrics is crucial not only because of the societal impact, but also because the time from beginning to end is short — just the nine months of pregnancy — making it easier to study. In other areas of medicine such as cancer or heart disease, studies can last for decades.
"The human body is a complex system," Bukowski said. "There are a lot of elements that interact with each other, which makes it very difficult to analyze in a traditional manner. It's difficult to draw conclusions from averages, and it's difficult to predict adverse outcomes."
Machine Learning Helps Pave the Way
We know from the computational side that there's a lot we can do to help," Gaither said. "At TACC, we know how to bring advanced computing to bear on this issue, including using data-driven science, mathematical models, and emerging computational techniques such as more advanced forms of machine learning."
"All of us, first and foremost, are motivated to improve medical care and outcomes for women and babies."
Currently, the team is using machine learning to analyze the risk of having an unplanned C-section. The hope is to improve the outcomes seen in labor and delivery using maternal characteristics recorded during labor to better quantify the risk of requiring an emergency C-section, according to Karl W. Schulz, a co-PI on the grant, a research associate professor for ICES, and an associate professor for Women's Health with Dell Med.
"This is a problem where we leverage risk factors and patient characteristics using data at a national scale over multiple years," Schulz said. The data used for this analysis is published by the Centers for Disease Control and Prevention (CDC) and provides vital statistics for all U.S. births, approximately four million per year.
Schulz said that machine learning techniques can be used to determine which patient factors are the best at predicting certain health risks by training and evaluating a variety of models, and assessing the accuracy of their results against available test data.
Modeling parameters from the CDC data are divided into two categories: those that are known during pregnancy versus those that are known during labor and delivery. Influential factors belonging to the former include maternal age, live birth order, diabetes, hypertension, and the number of previous cesareans.
Schulz said that moving forward, TACC's newly announced supercomputer, Frontera, is going to allow analysis on confidential HIPAA data and be "a great resource for research in computational health."
Data Challenges in Healthcare
There are four major data challenges in healthcare — access, quality, inconsistency, and integration. All data, whether it's from the CDC, Medicaid, electronic medical records, or private insurance, are going to have similar problems.

In terms of access, for example, researchers are unable to get data about mothers and babies from death records. A researcher might know that the mother died of complications from childbirth, but the records don't contain data about anything leading up to the complications or about the birth and post-partum period.
To help with this challenge, the team is partnering with the School of Public Health at the UT Texas Health Science Center at Houston to create a data architecture capable of housing large collections of heterogeneous types of health data, clinical records, and medical claims, among others.
"We're creating a large health data infrastructure with the UT School of Public Health," said Tomislav Urban of TACC, a key member of the team. "They have outgrown their capacity and would like to move the data to TACC for larger space, but also for analysis and reporting."
Urban has created a database, primarily from CDC data, that correctly maps data points to meta-fields and meta-values over a 10 year period from 2006 to 2016. The CDC data captures statistics from various states including vital statistics such as births, causes of death, weight gain during pregnancy, and cigarette smoking. There are about 300 different fields on these annual data sets.
"However, the agency de-identifies them, so they don't include any personal or geographical information," Urban said.
Mapping the fields to a common set of values, organizing the data, and cleaning the data is important because the team is looking for rare events, trying to create more accurate models and develop a more personalized look at the attributes of an individual, not just of a general population.
"All of us, first and foremost, are motivated to improve medical care and outcomes for women and babies," Gaither concluded.
"We believe this type of truly interdisciplinary team working together for this common goal leverages the diverse set of expertise, perspectives, and experiences that we all have, and is key to advancing the state of the art in health. While we have very different skill sets, we all have one thing in common: we either have been a patient in the past or will be one in the future."
Health informatics applies information technology and advanced computing to the field of healthcare. Other TACC-enabled health informatics projects include LungMAP, a detailed molecular atlas of developing lungs, and the Virtual Drug Discovery Portal, a graphical interface for identifying small molecules that bind to target proteins. Learn more about this growing research area: useta.cc/health